At Pelex we are dedicated to providing comprehensive fertility care that's tailored to your unique needs, whether you're seeking in-person consultations or prefer the convenience of telemedicine services.
THE PELEX PROMISE
With a team of experienced fertility specialists and cutting-edge technology, we're committed to delivering the highest standard of care to help you achieve your dream of starting or growing your family. Our compassionate and knowledgeable staff are here to guide you every step of the way, offering support, expertise, and personalized treatment plans designed to optimize your chances of success.
Learn more from Dr. Wolff
Pelex Services

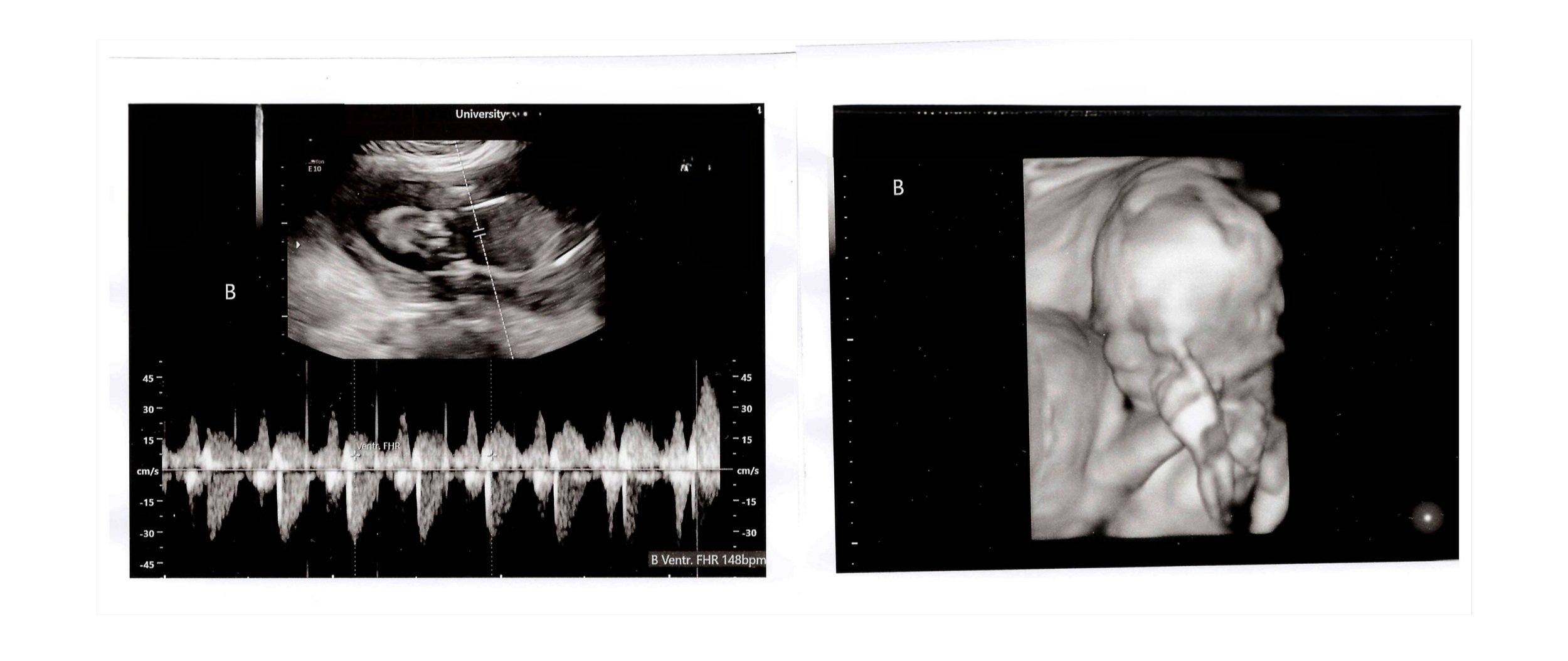
“I’m doing so well! 25 weeks and the boys were each measuring 1.4lbs at our sonogram last week. Couldn’t be happier!
Thank you all again! Miracle workers!!!”
Fertility Expert
Dr. Erin Wolff
Dr. Wolff obtained her Obstetrics and Gynecology residency training at Yale, where she received multiple awards for being the best physician and also the best surgeon. After residency, she was one of only two OB/GYNs in the country to receive a Reproductive Scientist Development Award, which allowed her to continue her work at one of the top fertility research labs in the world. Given her achievements as a physician, surgeon, and researcher, Dr. Wolff was accepted into the Reproductive Endocrinology and Infertility Fellowship in the Combined Federal Fellowship at Walter Reed Army Hospital and the NIH, where she was able to provide care to US Active Military and their dependents. After fellowship, she became the Head of the Unit on Reproductive and Regenerative Medicine at NIH, with a dual appointment at the National Institute of Child Health and Human Development and National Heart, Lung and Blood Institute, conducting basic, translational, and clinical research. While working at NIH, Dr. Wolff also worked part-time at the largest IVF practice in the country, where she performed thousands of IVF procedures and surgeries. In addition, she performed the first egg retrieval ever done at the NIH after she established NIH’s first fertility preservation program. She left the NIH to become the Chief Medical Officer of a startup company for genetics and women’s health before starting Pelex after her own difficult experiences with infertility.
Dr. Wolff is married to her med school sweetheart, Dr. Andy Wolff, and they have a son in college and a daughter in high school. In her spare time, she enjoys watching her kids play sports, spending time with family at the lake, trail rides on horseback, traveling, golfing, knitting, and baking.

In-Person Care
9826 Slide Rd #200, Lubbock, TX 79424